Mast Cell Diseases
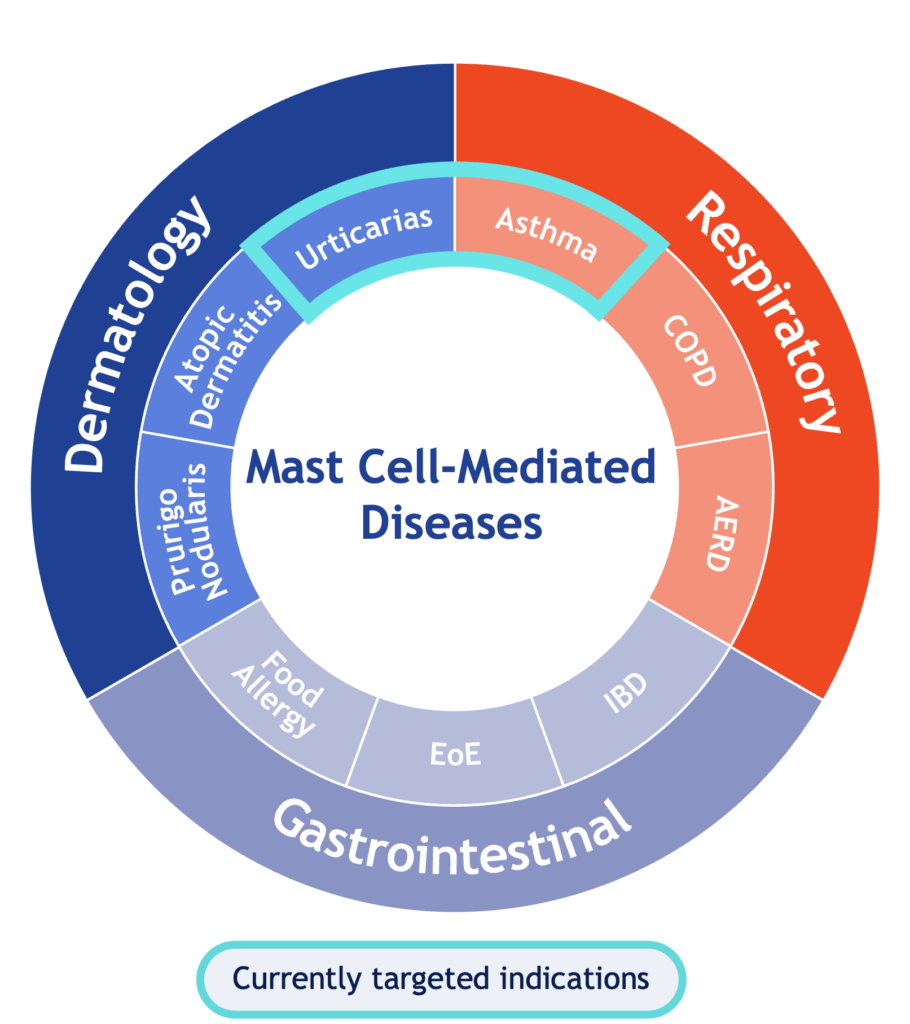
Mast cells play a central role in a diverse set of chronic immunological and inflammatory diseases, presenting numerous potential opportunities for briquilimab, including in chronic spontaneous urticaria (CSU), chronic inducible urticaria (CIndU), prurigo nodularis, eosinophilic esophagitis, allergic asthma, food allergy, chronic obstructive pulmonary disease (COPD) and inflammatory bowel disease.
Chronic Urticaria
Chronic Urticaria (CU) a recurring inflammatory condition of the skin lasting 6 weeks or more and is characterized by the development of itchy wheals (hives), angioedema, or both. CU can be classified as spontaneous (CSU) or inducible (CIndU). CSU occurs in the absence of an identifiable trigger, CIndU occurs in response to a defined and specific trigger that may include sun, heat, cold, or rubbing/scratching the skin.
CU is driven by the aberrant activation and degranulation of mast cells in skin. Activated mast cell release histamine, tryptase, tumor necrosis factor (TNF) and many other cytokines and cell mediators. Some of these mediators directly cause acute symptoms such as swelling, itching, edema or bronchoconstriction. Other mediators released by activated mast cells recruit other potent immune cells such as eosinophils, neutrophils, CD8+ T-cells and natural killer cells leading to further deepening of the aberrant inflammatory response. The full impact of CU, however, goes beyond the physical symptoms of the disease and is strongly associated with higher risk of suicide, depression, anxiety as well as reduced quality-of-life and ability to work.
Current treatment options for consist of small molecules such as antihistamines or leukotriene receptor antagonists targeting the symptoms of mast cell activation or a single biologic agent targeting IgE based activation. Many patients, especially those with moderate or severe CU, have limited or inadequate response to these agents and need new therapies to control their disease.
Allergic Asthma
Allergic asthma is a respiratory disease is triggered by exposure to environmental allergens such as pollen, pet fur or smoke leading to central infiltration of various immune mediators, cellular inflammation. Patients with allergic asthma often have an increased number of mast cells in the bronchi. Following aberrant activation and degranulation of mast cells, immune mediators are released which recruit eosinophils, Th2, and other cells into the airway that drive inflammation throughout all phases of the asthmatic response, and ultimately, lead to chronic airway remodeling. While recently approved biologic therapies have advanced the treatment of asthma patients with inadequate response to inhaled corticosteroids, long-acting beta-agonists and long-acting muscarinic antagonists, substantial unmet need remains, particularly for patients with allergic or T2-low asthma.